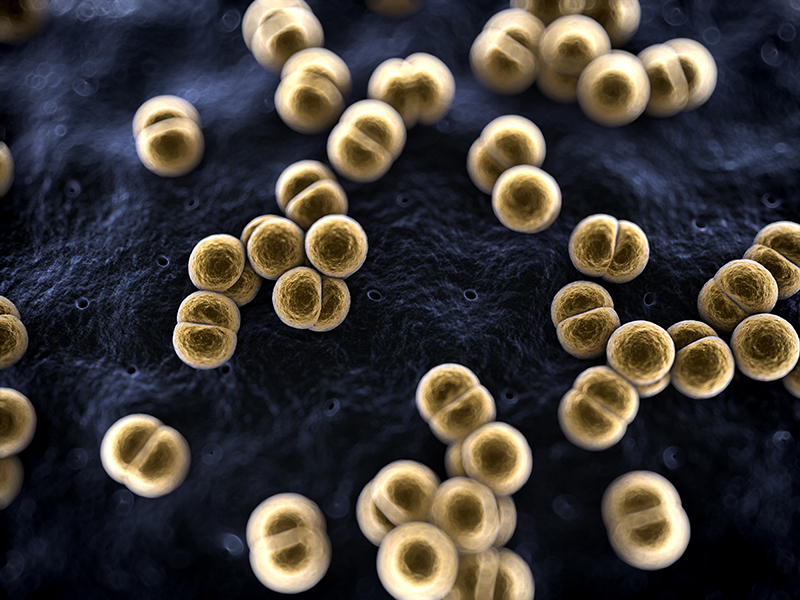
Neisseria meningitidis
Neisseria meningitidis or meningococcus is a Gram-negative, oxidasepositive, aerobic, coccal bacterium that appears microscopically under diplococcal arrangement. Strains are serogrouped on the basis of their capsular polysaccharides. The meningococci are one of the main causes of meningococcal meningitis.
Clinical characteristics: Meningococcal meningitis is a bacterial form of meningitis, a serious infection of the thin lining that surrounds the brain and spinal cord. It can cause severe brain damage and is fatal in 50% of cases if untreated.
The bacteria are transmitted from person-to-person through droplets of respiratory or throat secretions from carriers. Close and prolonged contact – such as kissing, sneezing or coughing on someone, or living in close quarters (such as a dormitory, sharing eating or drinking utensils) with an infected person (a carrier) – facilitates the spread of the disease. The average incubation period is 4 days, but can range between 2 and 10 days.
The most common symptoms are a stiff neck, high fever, sensitivity to light, confusion, headaches and vomiting. Even when the disease is diagnosed early and adequate treatment is started, 5% to 10% of patients die, typically within 24 to 48 hours after the onset of symptoms.
Diagnosis: Initial diagnosis of meningococcal meningitis can be made by clinical examination followed by a lumbar puncture showing a purulent spinal fluid. The bacteria can sometimes be seen in microscopic examinations of the spinal fluid. The diagnosis is supported or confirmed by growing the bacteria from specimens of spinal fluid or blood, by agglutination tests or by polymerase chain reaction (PCR). The identification of the serogroups and susceptibility testing to antibiotics are important to define control measures.
Treatment: Meningococcal disease is potentially fatal and should always be viewed as a medical emergency. Admission to a hospital or health centre is necessary, although isolation of the patient is not necessary. Appropriate antibiotic treatment must be started as soon as possible, ideally after the lumbar puncture has been carried out if such a puncture can be performed immediately. If treatment is started prior to the lumbar puncture it may be difficult to grow the bacteria from the spinal fluid and confirm the diagnosis.
A range of antibiotics can treat the infection, including penicillin, ampicillin, chloramphenicol and ceftriaxone.
Source: World Health Organization