Pneumocystis
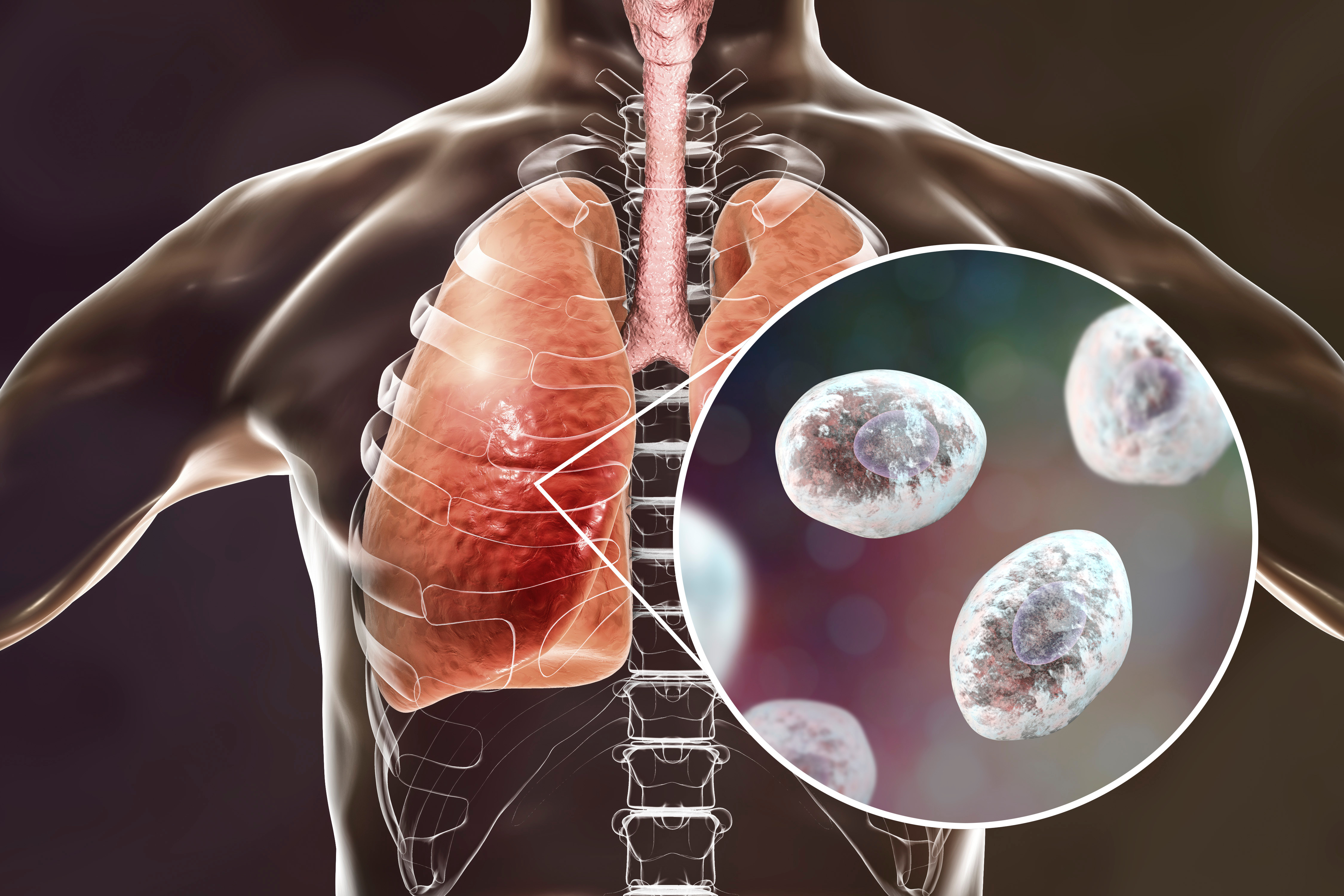
Pneumocystis jirovecii (P. jirovecii), formerly called P. carinii, is an atypical, opportunistic, extracellular, ubiquitous, unicellular, non-culturable, and pathogenic fungus that almost exclusively parasitizes the lungs of humans, affecting individuals with acquired immunodeficiency syndrome (AIDS) and patients with immunosuppression due to other causes, in which it produces pneumonia (Pneumocystis pneumonia (PCP) severe disease with a high morbidity and mortality rate.
Clinical characteristics: In most patients, pneumonitis progressing to pneumonia (PCP) occurs. There are at least 3 different patterns depending on the clinical manifestations or the immune status of the patient:
Patients with severe immunosuppression, such as children with severe undernourishment or congenital immunodeficiencies, and in HIV patients with very low CD4 counts. This pattern is characterized by hypoxemia with mild cough and dyspnea, most without fever. Children may progress to respiratory failure, with the presence of nasal flaring and intercostal retractions with cyanosis in severe cases.
Patients with unknown immunodeficiency, with sudden onset of hypoxemia, fever, cough, tachypnea, and dyspnea, which rapidly progresses to severe respiratory compromise.
Patients in whom antiretroviral therapy has been initiated and respiratory symptoms reappear after initial improvement (immune reconstitution syndrome or IRIS). This pattern has also been described in patients undergoing bone marrow transplantation.
In all cases, the clinical examination will show only dyspnea, when present, and dry cough, since pulmonary auscultation is usually normal. In a third of patients, basal crepitus may be auscultated, constituting a sign of poor prognosis, due to the great pulmonary involvement that they represent.
Diagnosis: In the clinical setting, the entity should be suspected in patients with respiratory symptoms, especially those with dyspnea, dry cough and hypoxemia with or without fever, and with the presence of risk factors such as: recurrent episodes of bacterial pneumonia, HIV infection with CD4 count < 200 cells/μL, high viral load, presence of oral candidiasis, weight loss and a history of PCP.
In the laboratory, elevated lactic dehydrogenase may be found in blood chemistry tests, which is a nonspecific marker of inflammation and alveolar injury, but its normal value makes the diagnosis of PCP less likely.
The microorganism is not culturable, so definitive diagnosis requires visualization of the fungus in respiratory specimens. This can be achieved by induced sputum (20%), tracheal aspiration (40%), bronchoalveolar lavage and bronchial brushing (75%), transbronchial biopsy (90%) and open biopsy (100%); However, the last 2 procedures are not recommended in patients with severe compromise, given the complications that may arise. The stains that allow the diagnosis are methenamine silver or Gomori staining and toluidine blue that stain the cystic forms; and Giemsa staining and the use of fluorescein-labeled monoclonal antibodies.
The search for the genetic material of the fungus by PCR has shown a sensitivity greater than 90% in bronchoalveolar lavage samples.
Treatment: The drug of choice for the treatment of PCP is trimethopin sulfamethoxazole (TMP/SMX). Initially, it is administered intravenously, but it can be given orally on an outpatient basis in patients with mild and moderate disease, and in those who do not have problems with its absorption. The use of corticosteroids is necessary in patients with a severe clinical picture, with oxygen saturation < 70 mmHg in arterial gases to air or alveolar-arterial difference > 35 mmHg. It should be started within the first 72 h of antibiotic initiation.