Clostridioides difficile
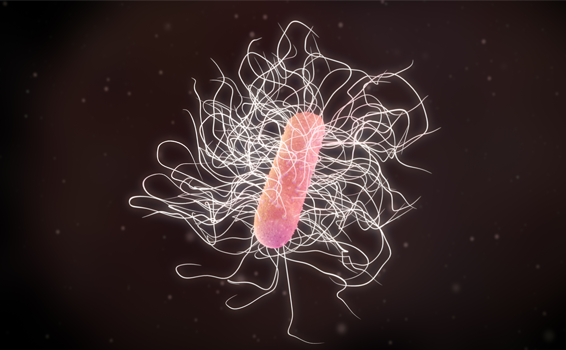
Clostridioides difficile more commonly known as Clostridium difficile is a gram-positive, strict anaerobic bacillus, forming spores that allow it to survive in water, soil and hospital environments, where it can remain for years. Initially, it was described in 1935 as a normal agent of the intestinal microbiota of healthy newborns.
Clinical characteristics: Its transmission by the fecal-oral route makes health personnel, medical objects and infected surfaces an important source of hospital-acquired infection, and is currently considered the main causative agent of nosocomial diarrhea associated with antibiotic treatment.
The clinical picture of C. difficile infection (CDI) can range from asymptomatic carriers to mild diarrhea, colitis or pseudomembranous colitis, and life-threatening toxic megacolon.
Thus, CDI is classified according to its severity. This classification is essential as it will determine the treatment that will be used.
Various virulence factors are associated with the development of the disease. The best known are toxins A and B, encoded by the genes tcdA and tcdB, respectively, and the binary toxin.
The presence of these toxins varies in the different strains of C. difficile and it is thought that the presence of one or more of them could act synergistically leading to more or less severe situations of C. difficile infection.
Diagnosis: The diagnosis of a CDI in a short time and with certainty is essential both in the management of the patient and in the taking of isolation measures, thus limiting the possibility of a nosocomial outbreak.
Accurate diagnosis includes different techniques from toxigenic culture to molecular techniques (such as PCR) and their use depends on the working algorithm established in the laboratory. It is still common to perform enzyme-linked immunoassay tests to detect the presence or absence of GDH (common antigen produced by C. difficile) and also the detection of toxins A and/or B. However, it should be borne in mind that the detection of GDH by EIA shows great variability in its performance, depending on the prevalence of CDI, with up to 15% of false negatives.
Currently, the use of molecular techniques, such as RT-PCR, which allow the direct detection of toxins A, B and binary toxin, are being implemented in working algorithms and recommended as a diagnostic method taking into account their high positive predictive value (80-95%) and negative predictive value (96-99%).
Treatment: The treatment to be indicated is based on the stratification of the severity of the CDI and paradoxically is with the prescription of antibiotics. Exposure to other antibiotics not selected to treat CDI should be avoided unless absolutely indicated. Continued use of antibiotics for infections other than CDI was associated with an increased risk of recurrence. Along with this, it is recommended to avoid the use of antiperistaltic agents as they can mask the symptoms and precipitate a toxic megacolon.